The results from the SAkuraStar clinical study demonstrated use of satralizumab as monotherapy reduced 55% risk of relapses in patients with NMOSD
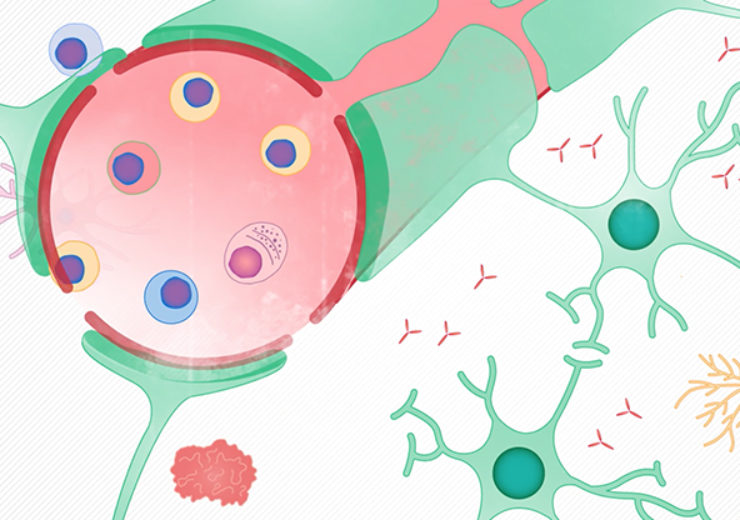
Image: Roche’s satralizumab significantly reduced relapse risk in second positive Phase III study. Photo: Courtesy of F. Hoffmann-La Roche Ltd.
Roche has announced positive results from a full pivotal Phase III study of satralizumab as a monotherapy for neuromyelitis optica spectrum disorder (NMOSD), a rare central nervous system disorder.
Satralizumab is an investigational humanised monoclonal antibody developed by Roche to target the IL-6 receptor. IL-6 is a cytokine that is said to trigger inflammation cascade, leading to damage in NMOSD.
According to the company, results from the previous Phase III study of satralizumab, as monotherapy and in combination with baseline therapy, indicated that the IL-6 inhibition would be an effective therapy for NMOSD.
Roche global product development head and chief medical officer Sandra Horning said: “While first described 125 years ago, the underlying biology of NMOSD has only recently been understood.
“The positive results from the pivotal SAkuraStar and SAkuraSky studies support the hypothesis that IL-6 plays a key role in this devastating disease that can take away people’s independence.
“We are encouraged by these results and look forward to working with regulators over the coming months to bring satralizumab to people living with NMOSD as soon as possible.”
SAkuraSky study evaluates satralizumab for NMOSD
NMOSD is a rare, chronic and debilitating autoimmune disease of the central nervous system that primarily damages the optic nerves and spinal cord, resulting in blindness, muscle weakness and paralysis.
SAkuraSky is a Phase III multicentre, randomised, double-blind, placebo-controlled study designed to assess the efficacy and safety of satralizumab added to baseline immunosuppressant therapy in patients with NMOSD.
The study, enrolling 95 patients of age between 20 and 70 years with NMOSD and 83 patients of age between 13 and 73, marks one of the largest clinical trial programmes undertaken for this rare disease.
The primary endpoint of the study was the time to first relapse as adjudicated by an independent review committee in the double-blind period, and the primary secondary endpoints included change in VAS score for pain and change in FACIT Fatigue score.
The results from the clinical trial, dubbed SAkuraStar study, showed that the use of satralizumab as monotherapy reduced 55% risk of relapses compared to placebo in patients with NMOSD.
University of Colorado neurology and ophthalmology professor Jeffrey Bennett said: “The positive phase III results for satralizumab, first as an add-on therapy and now as a monotherapy are exciting to see, and importantly, it achieved efficacy in a broad range of NMOSD patients, reflective of what we see in our everyday practice.
“Satralizumab targets the IL-6 receptor, potentially offering a novel treatment approach. Approved treatment options demonstrating favourable safety and efficacy in controlled clinical trials are urgently needed. Even one relapse may lead to blindness and debilitating motor dysfunction for people with NMOSD.”
